My sister texted me to let me know I need to post. So here it is.
This morning (or the smorning for some of you) I woke up early and Matt drove me to school two hours before classes started. I was in green surgical scrubs that I had quite the adventure finding yesterday (as it turns out, you cannot buy surgical scrubs in the school book store) and it was about 25 degrees out. But all of that was ok, because I was observing in the OR for the first time!
Our patient was a 40-something father of two from Chicago. He has Loeys-Dietz Syndrome, a disease of the arteries and presenting with cleft palate, wide-spread eyes and skeletal deformities. Patients with Loeys-Dietz have a high risk of death from aortic aneurysm rupture. Our patient had had a previous major surgery to repair some blood vessels and today the patient had a valve-sparing aortic root replacement for an aortic root aneurysm. (Here's a link to a video of the surgery in someone else.) This basically means that the surgeons opened his chest, cut out part of the aorta coming out of his heart taking the blood to the rest of his body, and sewed in a tube-like graft. Unfortunately, I didn't get to see any of the procedure because I had to go to class... but I did have a fabulous first glimpse into the operating room and started learning about anesthesia.
Our patient, V, was visiting with his wife and college-age daughter when Dr. M., his anesthesiologist and I walked in. Dr. M. explained what her part in the procedure would be, what it would feel like to "fall asleep," how many tubes he would have coming out of his nose and mouth when he woke up in the Intensive Care Unit after the surgery, and that the "margaritas" she would give him through his IV would keep him very warm and feeling good throughout his recovery. V didn't have many questions, but his wife wondered if the surgeons were planning to look at his other large blood vessels while they had him opened? No, they weren't. That wasn't on the consent form. V's daughter asked if he would have chest tubes in after the surgery? No, not like last time. This time he would have similar tubes coming out of his lower abdomen though. I started to feel sweaty and weak. The combination of the excitement of wearing the green scrubs and blue meshy cap, the fact that we were talking to V and his family, and the fact that it was rather warm in the pre-op space didn't really work for me at that moment. I took a second to take a few deep breaths and realize that my only job was to watch. I wasn't in charge of anyone's life, I wasn't the one who had no control over his life.
V asked to speak with the chaplain right after his wife and daughter went to the waiting room. While we waited for the chaplain to arrive I sat down next to V and learned that he was from Chicago, his son was still home finishing up his last week of high school before the holidays and that their flight was delayed several times on the way to Baltimore on Sunday. His daughter is studying journalism and wants to get involved in sports reporting.
Dr. M. is such a wonderful teacher. She was teaching Dr. B., a 3rd year resident who physically did most of the work under Dr. M's guidance and direction. When they were putting V to sleep she told me everything they were doing and made sure I could see at all times. When you're knocked-out with anesthesia you can't breathe for yourself, so you must be intubated with a breathing tube. This breathing tube went down into V's trachea, through his vocal cords and was attached to a ventilator. While they were getting things set, Dr. M. had me squeezing on the blue air bag to ventilate V manually. Dr. M. explained that I was breathing for V, that it was a very necessary part of the procedure to put his to sleep and keep him asleep through the surgery. "And all before my first class."
I watched everyone start draping and scrubbing V's body to prep him for the surgery while Dr. M. and Dr. B. administered drugs, sucked air and fluid out of his stomach and placed a central like in the large artery under his clavicle. I did not touch anything blue. Blue things are sterile and I'm not allowed to touch anything blue. Other than the air bag, I didn't touch anything at all.
Although I didn't get to see V's surgery, I am comfortable with the amount I did get to see today and I'm eager to go back and learn more. Dr. M. emailed me to let me know that the surgery ended at 5pm and was not without complications. They actually had to reopen his chest to address some ventricular fibrillation, quivering of the heart muscle instead of solid contractions. I'm eager to hear how V did coming out of the anesthesia and how his recovery turns out, and I'm equally eager to sign up for more shadowing... now that I have this school thing under control!
Tuesday, December 14, 2010
Tuesday, November 23, 2010
Hypochondriasis
Also known as Medical Students' Disease. I'm pretty sure I caught it.
It's finally Thanksgiving Break! Unfortunately my sniffing and sneezing is getting in the way of my relaxation. The problem is that I'm terrified to take something that might help me sleep, like NyQuil. NyQuil contains pseudoephedrine that helps to relieve nasal congestion by shrinking swollen nasal mucous membranes. Today we learned that the pseudoephedrine also causes an increase in the secretion of a "natural drug" produced by the body called norepinephrine. Norepinephrine directly increases the heart rate and therefore increases blood pressure.
Flashback 12 hours: Lecture 2, Case 3: 45 year old female with history of depression comes in with a cold and cough. You, the doctor, tell her to go home and take over-the-counter cough medicine. She takes 2 tablespoons of NyQuil. Two hours later she experiences cardiac arrest.
So, the problem was unfortunately the doctor didn't ask about other medications the patient might have been taking. This woman was taking medication for depression (MAO Inhibitors) that prevent the breakdown of norepinephrine. So, one medication (NyQuil) increases the release of norepinephrine that directly increases the heart rate and the other drug (for depression) prevents the break down of this "natural drug," further increasing its effect on the heart. Result: cardiac arrest.
No, I'm not taking anti-depression drugs. But, maybe the Tylenol I took earlier (for which the mechanism of action in the body is still debated) or the Mucinex I just took (that is so potent that it should only be taken every 12 hours) has some component that will interact with a component of NyQuil and stop my heart, or neurons, or liver....
The simultaneously fascinating and extremely scary thing about being a med student is learning about these things you never really considered before. This also includes learning about how cancer develops (which I'm more than terrified about), or how many things have to go right in order to have a healthy, genetically normal and successfully delivered baby (without damage to the very fragile brachial plexus).
I hope this hypochondriasis is only temporary, but I have a feeling it might last for about 3.5 more years.
It's finally Thanksgiving Break! Unfortunately my sniffing and sneezing is getting in the way of my relaxation. The problem is that I'm terrified to take something that might help me sleep, like NyQuil. NyQuil contains pseudoephedrine that helps to relieve nasal congestion by shrinking swollen nasal mucous membranes. Today we learned that the pseudoephedrine also causes an increase in the secretion of a "natural drug" produced by the body called norepinephrine. Norepinephrine directly increases the heart rate and therefore increases blood pressure.
Flashback 12 hours: Lecture 2, Case 3: 45 year old female with history of depression comes in with a cold and cough. You, the doctor, tell her to go home and take over-the-counter cough medicine. She takes 2 tablespoons of NyQuil. Two hours later she experiences cardiac arrest.
So, the problem was unfortunately the doctor didn't ask about other medications the patient might have been taking. This woman was taking medication for depression (MAO Inhibitors) that prevent the breakdown of norepinephrine. So, one medication (NyQuil) increases the release of norepinephrine that directly increases the heart rate and the other drug (for depression) prevents the break down of this "natural drug," further increasing its effect on the heart. Result: cardiac arrest.
No, I'm not taking anti-depression drugs. But, maybe the Tylenol I took earlier (for which the mechanism of action in the body is still debated) or the Mucinex I just took (that is so potent that it should only be taken every 12 hours) has some component that will interact with a component of NyQuil and stop my heart, or neurons, or liver....
The simultaneously fascinating and extremely scary thing about being a med student is learning about these things you never really considered before. This also includes learning about how cancer develops (which I'm more than terrified about), or how many things have to go right in order to have a healthy, genetically normal and successfully delivered baby (without damage to the very fragile brachial plexus).
I hope this hypochondriasis is only temporary, but I have a feeling it might last for about 3.5 more years.
Monday, November 22, 2010
My theory on studying and food
 During my freshmen year of college, I LOVED to snack on frosted raspberry poptarts while studying. I would use my Big Red Bucks and buy a package of 2 at the convenience store when leaving the all-you-can-eat dining hall and eat them for dessert while highlighting my textbooks. Ok fine, they were my second dessert, the soft serve ice cream bar was my first dessert at the end of my all-you-can-eat meal.
During my freshmen year of college, I LOVED to snack on frosted raspberry poptarts while studying. I would use my Big Red Bucks and buy a package of 2 at the convenience store when leaving the all-you-can-eat dining hall and eat them for dessert while highlighting my textbooks. Ok fine, they were my second dessert, the soft serve ice cream bar was my first dessert at the end of my all-you-can-eat meal. Sidenote: When I came home for Thanksgiving during my freshmen year, my best friend's mom (really my "second mom" growing up) asked, "Are your wisdom teeth acting up again?" She was referring to the fact that about 15 months before I had my wisdom teeth out and subsequently got an infection causing my cheeks to balloon for days. "No. It's called the Freshmen 15."
So. That was the end of the raspberry poptarts. However, I still have a problem with snacking while studying! I cannot stop eating when my brain is working so hard! Therefore, my theory is: Studying really hard is very similar to running a marathon (like I would know.....), you use energy rapidly and get very hungry very quickly.
Last week: Me: "Matt, we have no more chex-mix." Matt: "REALLY? I just bought that bag!"
Two days later: Me: "We are out of rosemary and garlic triscuits." Matt: "I know. You ate ALL the snacks."
I don't actually know if using your brain burns calories, but I did a tiny bit of research and found this article which is slightly off topic, but interesting: "The energy expenditure of using a “walk-and-work” desk for office workers with obesity" by James Levine and Jennifer Miller out of the Mayo Clinic. Hm... what a workplace that would be.
What I would do
The "Audience response questions" did not work very well. No one responded! haha
Truthfully, it's not fair of me to ask people what they would have done... it's a hard topic and it would not have been anonymous. In class, we voted with clickers and there was no way to tell who said what. But I'll tell you how I voted, and then what actually happened in these two real cases.
In the case of the newborn Down syndrome whose parents refuse the life saving surgery, I would
b. Apply for court appointed guardianship so that an operation can be performed to save the child’s life.
I think this would cover the legal aspect of going against the wishes of the parents and give the child a chance at life. What actually happened was:
e. Leave the child at hospital B to die under the care of the house staff and nurses
It was explained that this was the decision of the medical team involved. They felt this was the most ethical choice. It makes me really sad.
In the case of the 25 year old severely burned in a motor vehicle accident and wanted his doctors and nurses to end his life, I would
d. Request psychiatric consultation to declare the patient incompetent to make decisions regarding his own care
... with the caveat that I wouldn't be pushing for the consultation to automatically declare the patient incompetent, rather be trying to determine if the patent was competent enough to make the decision to end his life. My feelings are that I would want to be able to make my own decisions about my life and care if ever in such a painful, devastating and unbearable situation. Therefore, this man should be allowed to make his own decisions if he was competent enough to do so.
What actually happened was the b. Consider the patient incapable of requesting withdrawal of care and continue regardless of patient wishes. The patient, Dax Cowart, is famous in the medical ethics world. Should the patient have the right to die? Dax subsequently went on to get married, go to law school and fight for the rights of patients to choose their fate.
Truthfully, it's not fair of me to ask people what they would have done... it's a hard topic and it would not have been anonymous. In class, we voted with clickers and there was no way to tell who said what. But I'll tell you how I voted, and then what actually happened in these two real cases.
In the case of the newborn Down syndrome whose parents refuse the life saving surgery, I would
b. Apply for court appointed guardianship so that an operation can be performed to save the child’s life.
I think this would cover the legal aspect of going against the wishes of the parents and give the child a chance at life. What actually happened was:
e. Leave the child at hospital B to die under the care of the house staff and nurses
It was explained that this was the decision of the medical team involved. They felt this was the most ethical choice. It makes me really sad.
In the case of the 25 year old severely burned in a motor vehicle accident and wanted his doctors and nurses to end his life, I would
d. Request psychiatric consultation to declare the patient incompetent to make decisions regarding his own care
... with the caveat that I wouldn't be pushing for the consultation to automatically declare the patient incompetent, rather be trying to determine if the patent was competent enough to make the decision to end his life. My feelings are that I would want to be able to make my own decisions about my life and care if ever in such a painful, devastating and unbearable situation. Therefore, this man should be allowed to make his own decisions if he was competent enough to do so.
What actually happened was the b. Consider the patient incapable of requesting withdrawal of care and continue regardless of patient wishes. The patient, Dax Cowart, is famous in the medical ethics world. Should the patient have the right to die? Dax subsequently went on to get married, go to law school and fight for the rights of patients to choose their fate.
Tuesday, November 16, 2010
What would you do?
From Dr. M's lecture today on Medical Ethics:
Case 1: Audience response question
Newborn with Trisomy 21(Down syndrome) transferred from hospital A to hospital B. Unable to keep food down, vomiting solid and liquid foods. Duodenal atresia (small intestine malformation), complete blockage beyond stomach. Surgical recommendation to relieve obstruction.
Parents refuse, citing:
• poor future quality of life for child
• additional drain on family’s resources away from other children
• the child is “as God made him” and it is God’s will that the child should be allowed to die on its own without intervention
What would you do?
a. Refuse to accept the parents wishes: repair the small intestine
b. Apply for court appointed guardianship so that an operation can be performed to save the child’s life.
c. Send the child to die at home with its parents
d. Transfer the child back to die in the initial hospital (hospital A)
e. Leave the child at hospital B to die under the care of the house staff and nurses
f. Administer lethal doses of medication to the child to end its life quickly as an alternative to starvation and dehydration.
Case 2: Audience response question
25 year old military pilot involved in motor vehicle accident with father, both engulfed by flames. His memory of scene of accident:
"I was burned so severely and in so much pain that I did not want to live even in the early moments following the explosion. A man who heard my shouts for help came running down the road, I asked him for a gun. He said, 'Why?' I said, 'Canʼt you see I am a dead man? I am going to die anyway. I have got to put myself out of this misery.' In a very kind and compassionate caring way, he said, 'I canʼt do that.”
Patientʼs father dies en route to hospital. Throughout his hospitalization and rehabilitation, he asks his doctors and nurses to end his life because he is in unbearable pain and knows that he is blind and deformed.
What would you do?
a. Respect the patient’s wishes and administer a lethal dose of morphine and barbiturates
b. Consider the patient incapable of requesting withdrawal of care and continue regardless of patient wishes
c. Consider the patient incapable of making informed decisions and defer to closest relative: his mother
d. Request psychiatric consultation to declare the patient incompetent to make decisions regarding his own care
e. Transfer the patient to another burn treatment facility
Please include your reasoning for your answer(s).
Case 1: Audience response question
Newborn with Trisomy 21(Down syndrome) transferred from hospital A to hospital B. Unable to keep food down, vomiting solid and liquid foods. Duodenal atresia (small intestine malformation), complete blockage beyond stomach. Surgical recommendation to relieve obstruction.
Parents refuse, citing:
• poor future quality of life for child
• additional drain on family’s resources away from other children
• the child is “as God made him” and it is God’s will that the child should be allowed to die on its own without intervention
What would you do?
a. Refuse to accept the parents wishes: repair the small intestine
b. Apply for court appointed guardianship so that an operation can be performed to save the child’s life.
c. Send the child to die at home with its parents
d. Transfer the child back to die in the initial hospital (hospital A)
e. Leave the child at hospital B to die under the care of the house staff and nurses
f. Administer lethal doses of medication to the child to end its life quickly as an alternative to starvation and dehydration.
Case 2: Audience response question
25 year old military pilot involved in motor vehicle accident with father, both engulfed by flames. His memory of scene of accident:
"I was burned so severely and in so much pain that I did not want to live even in the early moments following the explosion. A man who heard my shouts for help came running down the road, I asked him for a gun. He said, 'Why?' I said, 'Canʼt you see I am a dead man? I am going to die anyway. I have got to put myself out of this misery.' In a very kind and compassionate caring way, he said, 'I canʼt do that.”
Patientʼs father dies en route to hospital. Throughout his hospitalization and rehabilitation, he asks his doctors and nurses to end his life because he is in unbearable pain and knows that he is blind and deformed.
What would you do?
a. Respect the patient’s wishes and administer a lethal dose of morphine and barbiturates
b. Consider the patient incapable of requesting withdrawal of care and continue regardless of patient wishes
c. Consider the patient incapable of making informed decisions and defer to closest relative: his mother
d. Request psychiatric consultation to declare the patient incompetent to make decisions regarding his own care
e. Transfer the patient to another burn treatment facility
Please include your reasoning for your answer(s).
Thursday, November 11, 2010
It's Fall!
They told me these 4 years will fly by. I won't believe it when I'm finally graduating with my M.D. After only 3 months, I fully realize the truth in that statement. I can't believe we're already into November! I LOVE the fall! While growing up, the fall = a new school year. In Olean, NY September meant leaves changing colors, crisp breezes and back-to-school shopping at the Outlets or in Buffalo with my mom and sisters. (which begs the question: if I'm still starting a new school year in the fall, why no back-to-school shopping with my mom and sisters?!?!)
 Anyway... here in Baltimore it doesn't seem like fall until well into November. So here we are! Finally. Last night, while studying for my metabolism exam (read: boring), I made (homemade!) hot chocolate, lit the Yankee candle that smells like apples and put on my favorite slippers. It was awesome!
Anyway... here in Baltimore it doesn't seem like fall until well into November. So here we are! Finally. Last night, while studying for my metabolism exam (read: boring), I made (homemade!) hot chocolate, lit the Yankee candle that smells like apples and put on my favorite slippers. It was awesome!
Shout-Out to Kristen and Kathy for getting me addicted to the homemade hot chocolate they give out at Christmas:
Much of the reason my life is flying by can be attributed to the pace of the curriculum. Our "blocks" are 5-8 days long. Meaning a new topic, new teachers, new section leaders, and a new style every week or two. Today we had a metabolism exam (a block I wasn't particularly fond of, mostly due to the lack of organization of the faculty... how can posting powerpoint slides be that difficult!?), and tomorrow we start genetics. Then next Friday, a week from tomorrow, we have our genetics test. WOW.
In addition to that science-y curriculum, we are at the climax of our clinical skills curriculum. The day after my Thanksgiving Break I will perform a head-to-toe physical evaluation on a standardized patient. Get ready! To prepare for this we went to the hospital this past Monday to interview an inpatient and do an abbreviated physical exam. This patient has lupus, an autoimmune disease where the body attacks it's own cells and tissues. The patient had severe connective tissue disorders that caused hardening of the skin and bones and kidney failure among other things. He was so wonderful to interview. He was patient, kind, and understanding of our inexperience. When we asked him to let us know if he felt uncomfortable while we were examining him, his quote was, "You're probably more uncomfortable doing this than I am." Check.
 Anyway... here in Baltimore it doesn't seem like fall until well into November. So here we are! Finally. Last night, while studying for my metabolism exam (read: boring), I made (homemade!) hot chocolate, lit the Yankee candle that smells like apples and put on my favorite slippers. It was awesome!
Anyway... here in Baltimore it doesn't seem like fall until well into November. So here we are! Finally. Last night, while studying for my metabolism exam (read: boring), I made (homemade!) hot chocolate, lit the Yankee candle that smells like apples and put on my favorite slippers. It was awesome!
Shout-Out to Kristen and Kathy for getting me addicted to the homemade hot chocolate they give out at Christmas:
Homemade Hot Chocolate Mix
Ingredients:
1 large can of Nestle Quick Choc. Mix (32 oz?)
1/2 bag confectioners sugar
11 oz container of non-dairy coffee creamer
8-10 qt. box dry milk (Sanalac brand is best)
Combine all ingredients together in LARGE bowl. Blend well.
Much of the reason my life is flying by can be attributed to the pace of the curriculum. Our "blocks" are 5-8 days long. Meaning a new topic, new teachers, new section leaders, and a new style every week or two. Today we had a metabolism exam (a block I wasn't particularly fond of, mostly due to the lack of organization of the faculty... how can posting powerpoint slides be that difficult!?), and tomorrow we start genetics. Then next Friday, a week from tomorrow, we have our genetics test. WOW.
In addition to that science-y curriculum, we are at the climax of our clinical skills curriculum. The day after my Thanksgiving Break I will perform a head-to-toe physical evaluation on a standardized patient. Get ready! To prepare for this we went to the hospital this past Monday to interview an inpatient and do an abbreviated physical exam. This patient has lupus, an autoimmune disease where the body attacks it's own cells and tissues. The patient had severe connective tissue disorders that caused hardening of the skin and bones and kidney failure among other things. He was so wonderful to interview. He was patient, kind, and understanding of our inexperience. When we asked him to let us know if he felt uncomfortable while we were examining him, his quote was, "You're probably more uncomfortable doing this than I am." Check.
Wednesday, November 3, 2010
Dia de los Muertos
 Today we finally honored the contributions of the donors that so selflessly gave their bodies. Some of my classmates put together a wonderful celebration that allowed us to reflect on death, healing and learning. A few people read poems, there was a violin performance, and two of my classmates sang The Only Exception by Paramore. I was truly touched by the offers of others, and finally had the opportunity and venue to say "Thank you" to the person I got to know so well. A moment of silence gave us the opportunity to write down a reflection and drop it in a bowl of water on a Dia de los Muertos altar.
Today we finally honored the contributions of the donors that so selflessly gave their bodies. Some of my classmates put together a wonderful celebration that allowed us to reflect on death, healing and learning. A few people read poems, there was a violin performance, and two of my classmates sang The Only Exception by Paramore. I was truly touched by the offers of others, and finally had the opportunity and venue to say "Thank you" to the person I got to know so well. A moment of silence gave us the opportunity to write down a reflection and drop it in a bowl of water on a Dia de los Muertos altar.Thank you for being the most amazing teacher, for letting me discover the details, and for giving me a completely new appreciation for life and the role of a physician.
Thursday, October 28, 2010
PETAs!!!
The week after Thanksgiving break will be exciting! We are going to take our practical clinical exam, including a full patient interview and a full physical exam (on a standardized patient actor). To prepare for this grand event, we've been learning the physical exam in sections: head and neck, lung, cardiovascular, abdominal, musculoskeletal, and neurologic exams.
There is a total of 104 things we must to during the 40 minutes we will have with the patient. Some will be ridiculously easy: wash hands, observe patient's general appearance... And most will be really interesting and fun: Inspect ear canals and tympanic membranes using otoscope... the problem is there are 104 of them that need to be done in order and properly.
The Physical Exam Teaching Associate program allows us to practice all aspects of the physical exam on real live people. Today I spend 1.5 hours with another student practicing the Neurological Exam on a PETA. It was fabulous! Below is the checklist for this portion of the exam.
So! If you would like to receive a FREE physical exam from someone who may or may not be able to identify findings, and almost certainly won't be able to explain why you have a bump there or can't follow my finger with your eyes or don't have a Babinski Reflex... please let me know! I'm willing to make house calls. :-) But seriously, I need to practice! This is only 38 of the 104 things I need to be able to do!
H. Psychiatric and Neurologic Mental Status Exam (9 items)
___ Observe level of consciousness: Awake and Alert?
Consciousness and Orientation:
___ Assess orientation: Asks patient: name, day, date, time, place and situation
___ Assess attention: Asks patient to recite days of week forward and backwards
Speech
___ Ask patient to name three objects :
___ Ask patient to repeat, “The sky is blue in Baltimore”.
___ Ask patient to point to the ceiling and point to the way out of the room.
___ Notes speech quality (e.g. clear/coherent; slurred, rambling)
___ Assess mood (predominant emotional state) and affect (emotional expression)
Mood and Thought:
___ Assess thought content and behavior.
J. Neurologic Exam (29 items)
Cranial nerves (10 items)
___ Check pupils and assesses for consensual response-bilaterally
___ Test visual fields; ask how many fingers are seen on each side (not total of both hands)
___ Extra-ocular: Ask to follow finger from center to left to right to center to up and to down.
___ Sensation: Touch quickly V1, V2, and V3 on each side
___ Ask patient to close eyes tightly, then open widely (observe forehead wrinkling). of face
___ Ask patient to show teeth
___ Rub fingers in each ear to assess hearing
___ Observe elevation of palate
___ Ask patient to protrude tongue
___ Test shoulder shrug strength bilaterally
Motor (5 items) - All are bilateral assessments
___ Check for pronator drift bilaterally
___ Check proximal arm strength at deltoid: arms in ‘chicken wing position- test one side at a time
___ Check finger extensor strength bilaterally
___ Check hip flexor strength bilaterally
___ Check dorsiflexion of foot strength bilaterally
Sensation (4 items) - All bilateral assessments
___ Fine touch: Use cotton tip on mid-arm, distal phalanx of index finger, mid-thigh, distal phalanx of great toe- (ask patient to close eyes)
___ Pain: use point of broken wooden shaft of cotton swab for pin-prick on mid-arm, distal phalanx of index finger, mid-thigh and distal phalanx of great toe
___ Vibration- use 128 or 256 Hz tuning fork on PIP joint of great toe bilaterally, counting to 10
___ Proprioception- moving great toe up or down
Reflexes (3 items) - All bilateral assessments
___ Strike tendon on one of biceps or brachioradialis bilaterally
___ Strike tendon on one of patella or ankle tendon bilaterally
___ Assess Babinski reflex, warning patient first of possible discomfort.
Coordination/Gait (7 items)
___ Perform finger to nose testing both sides using two points for each side- bilateral
___ Rapidly tap 5 times on thigh with each hand (rhythm and regularity)-bilateral
___ Ask patient to stand and walk distance of 10 feet (if possible)
___ Ask patient to stand with feet together, then close eyes (provide contact guard)
___ Ask patient to walk with one foot in front of the other (tandem walk).
___ Ask patient to stand on heels then stand on toes.
___ Alternate: heel to shin test-bilateral (may omit if performs all of walking/gait tasks)
There is a total of 104 things we must to during the 40 minutes we will have with the patient. Some will be ridiculously easy: wash hands, observe patient's general appearance... And most will be really interesting and fun: Inspect ear canals and tympanic membranes using otoscope... the problem is there are 104 of them that need to be done in order and properly.
The Physical Exam Teaching Associate program allows us to practice all aspects of the physical exam on real live people. Today I spend 1.5 hours with another student practicing the Neurological Exam on a PETA. It was fabulous! Below is the checklist for this portion of the exam.
So! If you would like to receive a FREE physical exam from someone who may or may not be able to identify findings, and almost certainly won't be able to explain why you have a bump there or can't follow my finger with your eyes or don't have a Babinski Reflex... please let me know! I'm willing to make house calls. :-) But seriously, I need to practice! This is only 38 of the 104 things I need to be able to do!
H. Psychiatric and Neurologic Mental Status Exam (9 items)
___ Observe level of consciousness: Awake and Alert?
Consciousness and Orientation:
___ Assess orientation: Asks patient: name, day, date, time, place and situation
___ Assess attention: Asks patient to recite days of week forward and backwards
Speech
___ Ask patient to name three objects :
___ Ask patient to repeat, “The sky is blue in Baltimore”.
___ Ask patient to point to the ceiling and point to the way out of the room.
___ Notes speech quality (e.g. clear/coherent; slurred, rambling)
___ Assess mood (predominant emotional state) and affect (emotional expression)
Mood and Thought:
___ Assess thought content and behavior.
J. Neurologic Exam (29 items)
Cranial nerves (10 items)
___ Check pupils and assesses for consensual response-bilaterally
___ Test visual fields; ask how many fingers are seen on each side (not total of both hands)
___ Extra-ocular: Ask to follow finger from center to left to right to center to up and to down.
___ Sensation: Touch quickly V1, V2, and V3 on each side
___ Ask patient to close eyes tightly, then open widely (observe forehead wrinkling). of face
___ Ask patient to show teeth
___ Rub fingers in each ear to assess hearing
___ Observe elevation of palate
___ Ask patient to protrude tongue
___ Test shoulder shrug strength bilaterally
Motor (5 items) - All are bilateral assessments
___ Check for pronator drift bilaterally
___ Check proximal arm strength at deltoid: arms in ‘chicken wing position- test one side at a time
___ Check finger extensor strength bilaterally
___ Check hip flexor strength bilaterally
___ Check dorsiflexion of foot strength bilaterally
Sensation (4 items) - All bilateral assessments
___ Fine touch: Use cotton tip on mid-arm, distal phalanx of index finger, mid-thigh, distal phalanx of great toe- (ask patient to close eyes)
___ Pain: use point of broken wooden shaft of cotton swab for pin-prick on mid-arm, distal phalanx of index finger, mid-thigh and distal phalanx of great toe
___ Vibration- use 128 or 256 Hz tuning fork on PIP joint of great toe bilaterally, counting to 10
___ Proprioception- moving great toe up or down
Reflexes (3 items) - All bilateral assessments
___ Strike tendon on one of biceps or brachioradialis bilaterally
___ Strike tendon on one of patella or ankle tendon bilaterally
___ Assess Babinski reflex, warning patient first of possible discomfort.
Coordination/Gait (7 items)
___ Perform finger to nose testing both sides using two points for each side- bilateral
___ Rapidly tap 5 times on thigh with each hand (rhythm and regularity)-bilateral
___ Ask patient to stand and walk distance of 10 feet (if possible)
___ Ask patient to stand with feet together, then close eyes (provide contact guard)
___ Ask patient to walk with one foot in front of the other (tandem walk).
___ Ask patient to stand on heels then stand on toes.
___ Alternate: heel to shin test-bilateral (may omit if performs all of walking/gait tasks)
Wednesday, October 27, 2010
Thank you Fourth Year!
Dear Amazing Fourth Year,
Thank you. Thank you for sitting me down and telling me what I need to know... what I need to know today, for this semester, for this year, and for this summer. And thank you for telling me that I don't need to worry about anything beyond that time frame right now.
Thank you for telling me that it's just safer to say "52 year old woman" rather than just "52 year old female" because an attending might ask, "Female person? Female dog?"
Thank you for offering to let me practice a head-to-toe physical exam on you (or a friend you beg to help us) so I can be ready for my practical exam in early December. I really can't do any of the systems without looking at the sheet (Heart rate then respiratory rate? The other way around? When do I listen to the lungs? When is the patient laying down, but elevated 30 degrees? What is jugular venous pressure and where do I look to see that it's normal?.... ya got me!)
Thank you for setting up times for me to go to the hospital and round with the attendings, residents and 4th years. I think it will be really helpful to see it all in action! And I can't imagine a better motivator than wearing my white coat in front of real live patients :)
Most of all, thank you for going through med school, even though none of your family went through it and you didn't know what to do or what to expect, because by watching and listening to you - I KNOW that it will all come together! Instead of having a list or 2 or 3 differentials or possible causes of the illness, I'll be able to list off 15 things when an attending or resident asks me for a differential diagnosis. And I'll be able to defend why each one might be the cause... and I'll know which tests, observations or questions about the patient's history would eliminate things from my list.
It's ok to be at the "one day at a time" phase right now. And I am suddenly really excited to learn this stuff about how cells work! I need to know how ion channels in cell membranes work... so I can understand how they make muscles contract... because certain drugs will alter these ion channels to increase heart rate or decrease heart rate. And I need to know that - because eventually I'll see a patient who is having a problem with her heart and I'll have to give her a drug. And I better know what drug will help her because then she might give me a hug and say thank you. And that will be a good day.
So thank you.
Sincerely,
Melissa
Thank you. Thank you for sitting me down and telling me what I need to know... what I need to know today, for this semester, for this year, and for this summer. And thank you for telling me that I don't need to worry about anything beyond that time frame right now.
Thank you for telling me that it's just safer to say "52 year old woman" rather than just "52 year old female" because an attending might ask, "Female person? Female dog?"
Thank you for offering to let me practice a head-to-toe physical exam on you (or a friend you beg to help us) so I can be ready for my practical exam in early December. I really can't do any of the systems without looking at the sheet (Heart rate then respiratory rate? The other way around? When do I listen to the lungs? When is the patient laying down, but elevated 30 degrees? What is jugular venous pressure and where do I look to see that it's normal?.... ya got me!)
Thank you for setting up times for me to go to the hospital and round with the attendings, residents and 4th years. I think it will be really helpful to see it all in action! And I can't imagine a better motivator than wearing my white coat in front of real live patients :)
Most of all, thank you for going through med school, even though none of your family went through it and you didn't know what to do or what to expect, because by watching and listening to you - I KNOW that it will all come together! Instead of having a list or 2 or 3 differentials or possible causes of the illness, I'll be able to list off 15 things when an attending or resident asks me for a differential diagnosis. And I'll be able to defend why each one might be the cause... and I'll know which tests, observations or questions about the patient's history would eliminate things from my list.
It's ok to be at the "one day at a time" phase right now. And I am suddenly really excited to learn this stuff about how cells work! I need to know how ion channels in cell membranes work... so I can understand how they make muscles contract... because certain drugs will alter these ion channels to increase heart rate or decrease heart rate. And I need to know that - because eventually I'll see a patient who is having a problem with her heart and I'll have to give her a drug. And I better know what drug will help her because then she might give me a hug and say thank you. And that will be a good day.
So thank you.
Sincerely,
Melissa
Monday, October 25, 2010
I whip my hair...
Sike naw.

Actually this is the version that plays in my house... for reasons you should probably know.

Awesome weekend:
Fri: dinner and drink out at a cute new bar: Diablita plus movie night with the hubby
Sat: school work then TWO parties: Amy's housewarming and Ryan's 30th Birthday
Sun: IMP Mentoring program football game - ending with kids vs. mentors... which we lost :(
Monday:
Ugh... I'm feeling more and more overwhelmed. It's not hard, it's just A LOT (see last post). In college or during TFA I was stretched, just as I am now. But, I didn't have a husband to come home to... and I really hate studying or doing cell physiology problem sets at night when we should be going for a walk, making dinner or just relaxing together.
I need to:
- Prioritize
- Be efficient
- Realize that I don't need to do everything or understand everything in the crazy amount of detail that is presented in class... I need to understand the big concepts... the forest, not the individual trees
- Call my mom (but remember not to make her worry that I'm eating or something crazy like that (I mean, come on, if there's one thing that I do very well every day... that's it, just get her to tell me it'll be ok!)
Thursday, October 21, 2010
Oops I did it again...
Dumb title, I know, but I feel bad I'm slacking on the blogging again. As it turns out, life gets busy. Anatomy is over and actually the block after anatomy is over! It's not as bad as it seems though, since our last block (Macromolecules) was only 8 days long. Did you ever hear the "medical school is like a trying to take a drink out of a fire hose analogy"...

I know how you feel.
<--
The last anatomy test went really well, and today's test turned out much better than I had expected. I'm trying really hard to stay away from the "just have to memorize this for the test" mindset and embrace the "I really want to understand the changes of the DNA double helix when adding more KCl to the buffer solution so I can apply the concepts to my career one day" pattern of thought. It's hard.
The hardest part is that often there isn't enough time to understand the material at a level beyond memorizing. Couple that with the fact that we're tested with multiple choice questions every day and you have a recipe for "know it for the test." Quizes, exams, the boards... we're always going to have to know the "answer." One of my classmates made the point that in the clinic, medicine really isn't a, b, c, d or all of the above. It's usually: how old is the patient, have they ever felt that pain before, does any one else in the family have experience with this symptom, what do they do for a living, what do they think is going on, what have they tried so far and has it helped, does anything make it worse? I wonder if there's a class on applying the multiple choice answer to the real life situation?
The good news is: my house is clean (including the shower and toilet!), the laundry is done and this weekend I'm spending time with Matt, my sister-in-law Amy, the Bmore crew and the child Matt and I are mentoring at the Kids vs. Mentors football game!

I know how you feel.
<--
The last anatomy test went really well, and today's test turned out much better than I had expected. I'm trying really hard to stay away from the "just have to memorize this for the test" mindset and embrace the "I really want to understand the changes of the DNA double helix when adding more KCl to the buffer solution so I can apply the concepts to my career one day" pattern of thought. It's hard.
The hardest part is that often there isn't enough time to understand the material at a level beyond memorizing. Couple that with the fact that we're tested with multiple choice questions every day and you have a recipe for "know it for the test." Quizes, exams, the boards... we're always going to have to know the "answer." One of my classmates made the point that in the clinic, medicine really isn't a, b, c, d or all of the above. It's usually: how old is the patient, have they ever felt that pain before, does any one else in the family have experience with this symptom, what do they do for a living, what do they think is going on, what have they tried so far and has it helped, does anything make it worse? I wonder if there's a class on applying the multiple choice answer to the real life situation?
The good news is: my house is clean (including the shower and toilet!), the laundry is done and this weekend I'm spending time with Matt, my sister-in-law Amy, the Bmore crew and the child Matt and I are mentoring at the Kids vs. Mentors football game!
Tuesday, October 12, 2010
The After Picture

 We had an awesome time at the Warrior Dash! It was so fun to be active, get muddy and drink beers on Sunday :) It wasn't easy... as confirmed by the fact that it's Tuesday and I'm still having trouble walking up steps... but I'd do it again.
We had an awesome time at the Warrior Dash! It was so fun to be active, get muddy and drink beers on Sunday :) It wasn't easy... as confirmed by the fact that it's Tuesday and I'm still having trouble walking up steps... but I'd do it again.Don't worry, 75% of those clothes did not come home with us! We were hosed down by a fire truck, seriously, and then changed into clean clothes to enjoy the festival. I even donated my muddy shoes to charity :)
Sunday, October 10, 2010
Warriors, Report for Battle!
Today is the Warrior Dash! A bunch of us are driving an hour into PA to run a 3.15 mile course set up with 13 obstacles... everything from climbing a wooden barricade to manuvering over cargo nets to crawling under barbed wire. Basically I'm terrified. I'm going with the group of friends that sends out the "let's do the Baltimore Marathon Relay!" or "Going for a run at 9am if anyone wants to join!" emails that I promptly delete. In the spirit of joining in on one of these "running" events I decided to actually sign up for this one. I mean, I won't actually have to run 3.15 miles straight... I get breaks to, um, climb over large stacks of hay. What was I thinking...
 I'm guessing mine is going to be more of a Warrior Slight Jog than a Warrior Dash.
I'm guessing mine is going to be more of a Warrior Slight Jog than a Warrior Dash.
 I'm guessing mine is going to be more of a Warrior Slight Jog than a Warrior Dash.
I'm guessing mine is going to be more of a Warrior Slight Jog than a Warrior Dash.
Friday, October 8, 2010
Anatomy lab is over
Today was our last day in the anatomy lab. One of my lab partners said it well: now that it's over it went by so fast...
We saw everything, and I mean everything, that makes up the human body: skin, muscles, nerves, vessels, fat, bones, organs, fascia (which is basically the term for "everything else that we can't really identify). It's so incredible how each person starts from a few small cells and develops into a fully functioning, thinking, expressive, emotional human. Over the past few weeks we've had a bunch of lectures on embryology and development - which makes me appreciate life even more.
I guess it wasn't so bad - and in fact - it was pretty awesome!
We saw everything, and I mean everything, that makes up the human body: skin, muscles, nerves, vessels, fat, bones, organs, fascia (which is basically the term for "everything else that we can't really identify). It's so incredible how each person starts from a few small cells and develops into a fully functioning, thinking, expressive, emotional human. Over the past few weeks we've had a bunch of lectures on embryology and development - which makes me appreciate life even more.
I guess it wasn't so bad - and in fact - it was pretty awesome!
Tuesday, October 5, 2010
When the first sentence is...
"The head must be detached from the vertebral column to allow a posterior approach to the cervical viscera" you know it's going to be a difficult dissection. The cervical viscera includes the pharynx, esophagus, larynx, and trachea with associated muscles, nerves and vessels. I guess we need to actually see how the nose and mouth are connected to the lungs and stomach.
We're nearing the end of our dissection of a human cadaver and although it's still ridiculously interesting to literally discover the large and small intricacies of the human body... the disarticulation of the head makes me ready to call it a day. Should I even mention that part of the dissection calls for bisection of the head? "Saw through the skull from superior to inferior." Awesome. And by awesome, I mean ugh. Keep in mind that our lady still has her nose, eyes (well, one of them remains in it's socket... we did eyes last week), lips and tongue. I'm pretty sure at this point I should NOT mention that I cut up beef into cubes and stir-fried them for dinner tonight.
We started with the chest in late August, then the abdomen, lower limbs, back, and upper limbs in September, and now the head and neck in October. Times flies when you're identifying (and really trying your best to memorize) every single muscle, never, artery, vein, bone and joint in the human body.

This picture from the BodyWorlds exhibit is actually pretty much what our body looks like after detaching one of the attachment points of many of the muscles. FYI: your forearm (elbow to wrist) has 19 muscles. Wow.
My good friend Jenny and I went to see the BodyWorlds exhibit in Baltimore in February 2008 and at the time she was getting her doctorate in Physical Therapy. As we walked through she kept saying, "You're going to learn all about all of this stuff when you dissect the body and you're going to love it!" I really wish we could go back through the exhibit together, as Jenny is a practicing Physical Therapist here in Baltimore now, and enjoy it again with this huge knowledge base I now have to draw from.
These are the muscles of facial expression (occipitofrontalis, orbicularis oculi, orbicularis oris, zygomaticus major and minor, buccinator, levator labii superioris, and depressor anguli oris). They are innervated by branchiomotor branches of cranial nerve VII... the oh so super fun facial nerve. ... Just in case you're taking a test on that soon :)

We're nearing the end of our dissection of a human cadaver and although it's still ridiculously interesting to literally discover the large and small intricacies of the human body... the disarticulation of the head makes me ready to call it a day. Should I even mention that part of the dissection calls for bisection of the head? "Saw through the skull from superior to inferior." Awesome. And by awesome, I mean ugh. Keep in mind that our lady still has her nose, eyes (well, one of them remains in it's socket... we did eyes last week), lips and tongue. I'm pretty sure at this point I should NOT mention that I cut up beef into cubes and stir-fried them for dinner tonight.
We started with the chest in late August, then the abdomen, lower limbs, back, and upper limbs in September, and now the head and neck in October. Times flies when you're identifying (and really trying your best to memorize) every single muscle, never, artery, vein, bone and joint in the human body.

This picture from the BodyWorlds exhibit is actually pretty much what our body looks like after detaching one of the attachment points of many of the muscles. FYI: your forearm (elbow to wrist) has 19 muscles. Wow.
My good friend Jenny and I went to see the BodyWorlds exhibit in Baltimore in February 2008 and at the time she was getting her doctorate in Physical Therapy. As we walked through she kept saying, "You're going to learn all about all of this stuff when you dissect the body and you're going to love it!" I really wish we could go back through the exhibit together, as Jenny is a practicing Physical Therapist here in Baltimore now, and enjoy it again with this huge knowledge base I now have to draw from.
These are the muscles of facial expression (occipitofrontalis, orbicularis oculi, orbicularis oris, zygomaticus major and minor, buccinator, levator labii superioris, and depressor anguli oris). They are innervated by branchiomotor branches of cranial nerve VII... the oh so super fun facial nerve. ... Just in case you're taking a test on that soon :)

Congratulations Rob and Val!
One million congratulations to my cousin Robert and his high school sweetheart! Here is the crazy creative proposal video. Enjoy :)


Saturday, October 2, 2010
And we're back!
Wow, it's been too long! (Diana - I don't know how you get a post in EVERY day!!! Good work!)
This past week as been super busy, but really awesome! Some of the highlights:
- Last weekend was fun filled with Matt's high school's Homecoming football game, a really great housewarming party in Alexandria, VA for wonderful friends, and a good-bye taco themed potluck for a girlfriend moving to Ohio.
- Second anatomy exam went really well!
- Practice musculoskeletal exam with a standardized patient actor - super helpful in learning how to do a physical exam and get comfortable talking to patients
- Tutoring a Dunbar High School student - which didn't actually go super well... but at least he knows I don't play! He WILL be passing his classes this year. All of them!
- Practice pediatric interview for a 6 month old well-baby visit! It was awesome to have children running around our simulation center (rows of exam rooms set up for us to practice in). Interviewing this new mother and watching her with her baby really helped ground what we are learning each week.
- Quick trip to Harrisburg to see my mom, Bridget, Mike and their new baby Juliana!
So, I will really try much harder to keep up to date with this blog. I do want to describe what we are doing in lab: dissecting the head and neck. We finished with the upper and lower limbs - which means that 80% of her muscles are hanging by one of their tendons to her body - and moved on to our last 2 week block of the super complicated head and neck.
Tuesday's post should have been: "What did you do today?" "Oh, I skinned a head."
Wednesday's post should have been: "Today we sawed the skull open and took out the brain."
Clearly it has been an interesting week.
This past week as been super busy, but really awesome! Some of the highlights:
- Last weekend was fun filled with Matt's high school's Homecoming football game, a really great housewarming party in Alexandria, VA for wonderful friends, and a good-bye taco themed potluck for a girlfriend moving to Ohio.
- Second anatomy exam went really well!
- Practice musculoskeletal exam with a standardized patient actor - super helpful in learning how to do a physical exam and get comfortable talking to patients
- Tutoring a Dunbar High School student - which didn't actually go super well... but at least he knows I don't play! He WILL be passing his classes this year. All of them!
- Practice pediatric interview for a 6 month old well-baby visit! It was awesome to have children running around our simulation center (rows of exam rooms set up for us to practice in). Interviewing this new mother and watching her with her baby really helped ground what we are learning each week.
- Quick trip to Harrisburg to see my mom, Bridget, Mike and their new baby Juliana!
So, I will really try much harder to keep up to date with this blog. I do want to describe what we are doing in lab: dissecting the head and neck. We finished with the upper and lower limbs - which means that 80% of her muscles are hanging by one of their tendons to her body - and moved on to our last 2 week block of the super complicated head and neck.
Tuesday's post should have been: "What did you do today?" "Oh, I skinned a head."
Wednesday's post should have been: "Today we sawed the skull open and took out the brain."
Clearly it has been an interesting week.
Monday, September 20, 2010
Just another Monday night
Order Chinese Food - Check 
Matt irons shirts for the week - Check Melissa tries to figure out the brachial plexus of nerves - eh...
Melissa tries to figure out the brachial plexus of nerves - eh...
Justin Bieber on repeat (every other song) - Check The Band Perry on repeat (every other song) - Check
The Band Perry on repeat (every other song) - Check 

Matt irons shirts for the week - Check
 Melissa tries to figure out the brachial plexus of nerves - eh...
Melissa tries to figure out the brachial plexus of nerves - eh...
Justin Bieber on repeat (every other song) - Check
 The Band Perry on repeat (every other song) - Check
The Band Perry on repeat (every other song) - Check 
Friday, September 17, 2010
Good News, Bad News
The Good News:
Bill Ferguson, fellow Teach For America alum, tireless advocate, and all around great human being , won the 46th District Maryland State Senate Democratic Primary! He beat out a guy who held the job for 27 years (or something like that) by utilizing his network and social media to get the young and thriving city involved. I'm really excited about what this means for the future of Baltimore City, specifically the school system and the kids. Baltimore's Time is Now!
Learn ab out Bill's goals, energy and commitment to the people of Baltimore City here.
out Bill's goals, energy and commitment to the people of Baltimore City here.
Watch his reaction to the win here.
The Bad News:
There was a shooting in Johns Hopkins Hospital yesterday. A patient's son shot his mother's doctor, killed his mother and then killed himself.
Ironically, last year's season finale of Grey's Anatomy that was already set to air last night (next week is the season premier) depicted essentially the same scenario: Distraught and frustrated patient unhappy with his loved one's care shoots the doctor. Here is a quick post: 'Grey's gets warning after Johns Hopkins shooting' from CNN's The Marquee Blog.
Honestly, this frustrates me. Baltimore has a bad rep. Gangs, drugs, the streets, the corners. This extremely unfortunate and shocking incident actually has nothing to do with why Baltimore has been labeled "rough," yet will inevitably add to the stereotype that Baltimore is an unsafe place to live and work. I don't feel unsafe at all. As my dad frequently reminds me, I can't get too comfortable and always need to be aware, but overall, I am not fearful for my health, safety or life. I'm not afraid to walk home from school, enjoy the parks around campus, or to ride the city bus system. I love Baltimore and I'm frustrated that the events of yesterday might be linked to the crime and violence that plagues some of our neighborhoods instead of seen as a situation that could have happened at any hospital in any city.
Baltimore does have issues that need to be addressed. There is crime and there are gangs. But thankfully we also have hope, we BELIEVE that Baltimore's Time is Now. The problems are not too big to fix as long as we are working at them from every angle: the school system, the health of our small businesses, the development of the neighborhoods as well as the waterfront, the health care system, the homeless population...
Part of the reason I joined Teach For America is because the vision statement includes the reality that not all teachers will stay in teaching. We, in fact, don't want all teachers to stay in the classroom, we want people to become inspired by the problems facing our most precious youth and then go fix them. We want Bill Ferguson to fight for our school system in the Maryland State Senate and we want good doctors that will care for our kids and families that have been underserved for generations. I hope that the doctors, nurses and all of the hospital faculty, the current medical school students and especially the prospective medical students that were interviewing yesterday know that Baltimore is not unsafe. The people of Baltimore need quality health care and deserve quality doctors that are comfortable living and working in Baltimore City.
My heart goes out to the doctor that was injured yesterday. I hope that he and his family are able to recover and heal with the support and love of the Johns Hopkins and Baltimore City communities.
Bill Ferguson, fellow Teach For America alum, tireless advocate, and all around great human being , won the 46th District Maryland State Senate Democratic Primary! He beat out a guy who held the job for 27 years (or something like that) by utilizing his network and social media to get the young and thriving city involved. I'm really excited about what this means for the future of Baltimore City, specifically the school system and the kids. Baltimore's Time is Now!
Learn ab
 out Bill's goals, energy and commitment to the people of Baltimore City here.
out Bill's goals, energy and commitment to the people of Baltimore City here.Watch his reaction to the win here.
The Bad News:
There was a shooting in Johns Hopkins Hospital yesterday. A patient's son shot his mother's doctor, killed his mother and then killed himself.
Ironically, last year's season finale of Grey's Anatomy that was already set to air last night (next week is the season premier) depicted essentially the same scenario: Distraught and frustrated patient unhappy with his loved one's care shoots the doctor. Here is a quick post: 'Grey's gets warning after Johns Hopkins shooting' from CNN's The Marquee Blog.
Honestly, this frustrates me. Baltimore has a bad rep. Gangs, drugs, the streets, the corners. This extremely unfortunate and shocking incident actually has nothing to do with why Baltimore has been labeled "rough," yet will inevitably add to the stereotype that Baltimore is an unsafe place to live and work. I don't feel unsafe at all. As my dad frequently reminds me, I can't get too comfortable and always need to be aware, but overall, I am not fearful for my health, safety or life. I'm not afraid to walk home from school, enjoy the parks around campus, or to ride the city bus system. I love Baltimore and I'm frustrated that the events of yesterday might be linked to the crime and violence that plagues some of our neighborhoods instead of seen as a situation that could have happened at any hospital in any city.
Baltimore does have issues that need to be addressed. There is crime and there are gangs. But thankfully we also have hope, we BELIEVE that Baltimore's Time is Now. The problems are not too big to fix as long as we are working at them from every angle: the school system, the health of our small businesses, the development of the neighborhoods as well as the waterfront, the health care system, the homeless population...
Part of the reason I joined Teach For America is because the vision statement includes the reality that not all teachers will stay in teaching. We, in fact, don't want all teachers to stay in the classroom, we want people to become inspired by the problems facing our most precious youth and then go fix them. We want Bill Ferguson to fight for our school system in the Maryland State Senate and we want good doctors that will care for our kids and families that have been underserved for generations. I hope that the doctors, nurses and all of the hospital faculty, the current medical school students and especially the prospective medical students that were interviewing yesterday know that Baltimore is not unsafe. The people of Baltimore need quality health care and deserve quality doctors that are comfortable living and working in Baltimore City.
My heart goes out to the doctor that was injured yesterday. I hope that he and his family are able to recover and heal with the support and love of the Johns Hopkins and Baltimore City communities.
Sunday, September 12, 2010
Finance... I mean Muppets
So, Matt told me he would write a few posts about the "Finances of Medical School" this weekend. At 10:30 pm on Sunday night this is what he turned in.
 He argued that instead of making everyone's eyes glaze over with boredom, he would hopefully be providing them with a chuckle on Monday morning. Questionable. Enjoy.
He argued that instead of making everyone's eyes glaze over with boredom, he would hopefully be providing them with a chuckle on Monday morning. Questionable. Enjoy.
 He argued that instead of making everyone's eyes glaze over with boredom, he would hopefully be providing them with a chuckle on Monday morning. Questionable. Enjoy.
He argued that instead of making everyone's eyes glaze over with boredom, he would hopefully be providing them with a chuckle on Monday morning. Questionable. Enjoy.Test Shmest
The first few weeks of school were a bit stressful. I didn't know what to expect, how to study, how long to study, or how deep to get into the material. Not wanting to give up my social activities or this newly-wed time in my life, I was carrying out a nice little balancing act. After the first anatomy test on Friday, I can confidently say that it's doable! I wanted to be over-prepared for the first exam, so I gave up some time with family and friends to study. Although I'm glad I was super ready for the test, I now realize that the world will not fall apart if I put down Gray's Anatomy and board a Pirate Ship with my friends (which I did miss out on... tear).
Some quick study tips:
1. Prepare for lecture by reading the notes, looking up crazy names of bones and ligaments, and finding pictures the structures I will learn about the next day.
2. Be efficient. By using the hours during the day to study, I am able to make dinner, walk to the store, and enjoy some QT with Matt at night. Sometimes I get out of class at 1pm - leaving 5 or 6 more hours to color code pictures of arteries and veins.
3. When studying, don't just do the reading to "check it off" my To Do List. Actually memorizing and learning structures, attachments, and functions while reading is more efficient than reading and then going though it all over again to actually learn it.
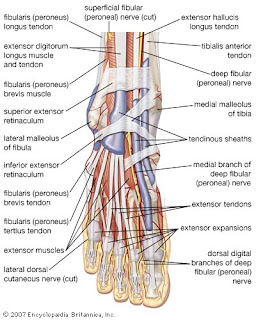
(Who knew the foot was so complicated?!)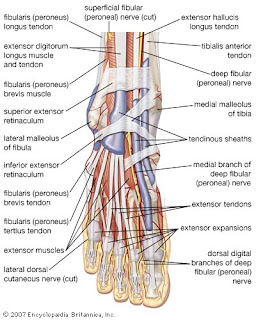
4. Plan! If I create a study plan for each day, each week, or each test then it's easier to stay ahead of the game and not feel overwhelmed!
5. Prioritize - not only what to study, but for how long to study that topic or those details. If something is super complicated, I'm going to need to spend more time on it... but how important are the tiny details of that complicated topic versus another topic I haven't even looked at!?
It's nice to know that hard work does pay off, as usual. It doesn't hurt that there were 8 extra credit points at the end of the test... "Is this medical school or eighth grade?!?!"... not that I'm complaining :-)
Some quick study tips:
1. Prepare for lecture by reading the notes, looking up crazy names of bones and ligaments, and finding pictures the structures I will learn about the next day.
2. Be efficient. By using the hours during the day to study, I am able to make dinner, walk to the store, and enjoy some QT with Matt at night. Sometimes I get out of class at 1pm - leaving 5 or 6 more hours to color code pictures of arteries and veins.
3. When studying, don't just do the reading to "check it off" my To Do List. Actually memorizing and learning structures, attachments, and functions while reading is more efficient than reading and then going though it all over again to actually learn it.
(Who knew the foot was so complicated?!)
4. Plan! If I create a study plan for each day, each week, or each test then it's easier to stay ahead of the game and not feel overwhelmed!
5. Prioritize - not only what to study, but for how long to study that topic or those details. If something is super complicated, I'm going to need to spend more time on it... but how important are the tiny details of that complicated topic versus another topic I haven't even looked at!?
It's nice to know that hard work does pay off, as usual. It doesn't hurt that there were 8 extra credit points at the end of the test... "Is this medical school or eighth grade?!?!"... not that I'm complaining :-)
Wednesday, September 8, 2010
Hummus on my notes
There is hummus on my urogenital triangle notes, spaghetti sauce on a drawing of the entire supply of blood to the foregut, midgut and hindgut, and ice cream on my To Do List. This must mean there is a test coming up. I am really looking forward to the day where I can eat a meal without Gray's Anatomy.
On a similar note, my husband made a comment to a bunch of friends the other night. After talking about how med school is or is not like Grey's Anatomy he says, "So, I didn't talk with Melissa about this yet, but guys, she has a book called Gray's Anatomy on her desk! I laugh every time I see it! It's crazy it's got the same name as the show!" Blank stares. Wow. He clearly should have brought that up with me before announcing it to the group.
When retelling that story to a classmate, she says, "He laughs when he sees it, I have quite a different visceral reaction when I see it!"
And on a completely different note, we did get our white coats today! And of course we had to buy them ourselves... (the school will give us ones at the end of the year apparently). So this video is included simply to note that eventually (I'm hoping after anatomy) there will be time to change the words to popular rap songs and make music videos.
On a similar note, my husband made a comment to a bunch of friends the other night. After talking about how med school is or is not like Grey's Anatomy he says, "So, I didn't talk with Melissa about this yet, but guys, she has a book called Gray's Anatomy on her desk! I laugh every time I see it! It's crazy it's got the same name as the show!" Blank stares. Wow. He clearly should have brought that up with me before announcing it to the group.
When retelling that story to a classmate, she says, "He laughs when he sees it, I have quite a different visceral reaction when I see it!"
And on a completely different note, we did get our white coats today! And of course we had to buy them ourselves... (the school will give us ones at the end of the year apparently). So this video is included simply to note that eventually (I'm hoping after anatomy) there will be time to change the words to popular rap songs and make music videos.

Tuesday, August 31, 2010
You can live without a stomach
This week we started dissecting the abdomen. We cut through all the layers of muscle holding our abdominal wall in place and protecting our organs, including the rectus abdominis (yeah six pack!), and several layers on the side like the external obliques, internal obliques and transversus abdominis muscles (yeah new words!).

Today, we started looking for the liver, stomach, spleen, pancreas, gall bladder and the veins and arteries running to and from these organs. Well.... to make a long story short: SHE HAS NO STOMACH! Crazy. Luckily, a wonderful thoracic surgeon happened to be in lab today and described the full gastrectomy that removed her stomach, spleen and the greater omentum that covers these organs. The pictures below helps to explain how the surgeons removed her stomach and hooked up her esophagus to her small intestine. Needless to say, we had a rough time in lab identifying all of the abdominal viscera because everything was shifted, reconnected and unexpected!

Here is a blog entry from a person living with a full gastrectomy: Living with a Gastrectomy: One Researcher's Experience.

Today, we started looking for the liver, stomach, spleen, pancreas, gall bladder and the veins and arteries running to and from these organs. Well.... to make a long story short: SHE HAS NO STOMACH! Crazy. Luckily, a wonderful thoracic surgeon happened to be in lab today and described the full gastrectomy that removed her stomach, spleen and the greater omentum that covers these organs. The pictures below helps to explain how the surgeons removed her stomach and hooked up her esophagus to her small intestine. Needless to say, we had a rough time in lab identifying all of the abdominal viscera because everything was shifted, reconnected and unexpected!

Here is a blog entry from a person living with a full gastrectomy: Living with a Gastrectomy: One Researcher's Experience.
Friday, August 27, 2010
Hey Med School! I thought that was you!
Thank god for clinical correlation lectures, teamwork in the anatomy lab, simulation centers, and observations of the patient interview! I'm writing this today... but it was actually yesterday that made me say, "YES! This is why I'm here!" Everything we had been learning about and dissecting in the thorax started to make sense and became relevant medically.
Dr. Yang, a top thoracic surgeon, did some show-and-tell about common, and crazy, surgeries of the lungs and heart. He gave the history of the surgery (they used to fill an empty lung sac with ping pong balls) and then gave us the run down of how the problems are fixed now. The amazingly cool part was that I followed what he was saying!!! I'm sure he didn't use every medical word he could have - but he did describe how the internal thoracic artery running just laterally to the sternum can be removed and used in coronary artery replacement surgery to repair the blood vessel that supplies blood to the heart muscle itself. Anyway... Dr. Yang's lecture made me feel like I was finally learning something :)
Working on any team is a challenge, and in anatomy lab, we are working on a team standing over a cadaver, dissecting tiny nerve in a rather small thorax. Sometimes there are too many cooks in the kitchen (yes, we wear white aprons!). Yesterday (and actually today also) we worked so well together! We found and cleaned off the aortic arch and the branches to the rest of the head and neck, we found both vagus nerves, the carotid arteries, and many other really cool structures! The excitement and cohesion were palpable (as were the arthritic vertebra).
The simulation center did not disappoint. First we were taught and practiced CPR on an adult, child and infant mannequins (compressions should be 100 times per minute, or to the song Stayin' Alive, demonstrated here in The Office). Then we saw how use a laryngoscope to insert a breathing tube into a patient along with the fiberoptic bronchoscope that's used to visualize a patient's trachea, bronchi and lungs. The last station introduced us to Sim Man, a breathing mannequin that has a medical problem and responds to your attempt to fix it. He had a collapsed lung and we practiced inserting a needle between the ribs (intercostal spaces) to allow the air to escape! As of today, I can't imagine doing that to an actual patient in distress, but Sim Man was good practice :)
along with the fiberoptic bronchoscope that's used to visualize a patient's trachea, bronchi and lungs. The last station introduced us to Sim Man, a breathing mannequin that has a medical problem and responds to your attempt to fix it. He had a collapsed lung and we practiced inserting a needle between the ribs (intercostal spaces) to allow the air to escape! As of today, I can't imagine doing that to an actual patient in distress, but Sim Man was good practice :)
Lastly, we observed a doctor interview a patient to learn proper communication techniques. This completely rounded out the day that made med school real. This was a 57 year old woman with bone marrow cancer. She told her story from beginning to end over 45 minutes. It was clear that she placed a lot of trust in Dr. Shochet, and that she respected him. I feel grateful to have these experiences to help me learn how to be a compassionate and competent doctor.
And after a long day, I even got some quality time with my husband! Of course, knowing that I hadn't yet showered after spending a good 4 hours in the anatomy lab, he did say, "Um, you smell a little bad..."
Dr. Yang, a top thoracic surgeon, did some show-and-tell about common, and crazy, surgeries of the lungs and heart. He gave the history of the surgery (they used to fill an empty lung sac with ping pong balls) and then gave us the run down of how the problems are fixed now. The amazingly cool part was that I followed what he was saying!!! I'm sure he didn't use every medical word he could have - but he did describe how the internal thoracic artery running just laterally to the sternum can be removed and used in coronary artery replacement surgery to repair the blood vessel that supplies blood to the heart muscle itself. Anyway... Dr. Yang's lecture made me feel like I was finally learning something :)
Working on any team is a challenge, and in anatomy lab, we are working on a team standing over a cadaver, dissecting tiny nerve in a rather small thorax. Sometimes there are too many cooks in the kitchen (yes, we wear white aprons!). Yesterday (and actually today also) we worked so well together! We found and cleaned off the aortic arch and the branches to the rest of the head and neck, we found both vagus nerves, the carotid arteries, and many other really cool structures! The excitement and cohesion were palpable (as were the arthritic vertebra).
The simulation center did not disappoint. First we were taught and practiced CPR on an adult, child and infant mannequins (compressions should be 100 times per minute, or to the song Stayin' Alive, demonstrated here in The Office). Then we saw how use a laryngoscope to insert a breathing tube into a patient
 along with the fiberoptic bronchoscope that's used to visualize a patient's trachea, bronchi and lungs. The last station introduced us to Sim Man, a breathing mannequin that has a medical problem and responds to your attempt to fix it. He had a collapsed lung and we practiced inserting a needle between the ribs (intercostal spaces) to allow the air to escape! As of today, I can't imagine doing that to an actual patient in distress, but Sim Man was good practice :)
along with the fiberoptic bronchoscope that's used to visualize a patient's trachea, bronchi and lungs. The last station introduced us to Sim Man, a breathing mannequin that has a medical problem and responds to your attempt to fix it. He had a collapsed lung and we practiced inserting a needle between the ribs (intercostal spaces) to allow the air to escape! As of today, I can't imagine doing that to an actual patient in distress, but Sim Man was good practice :)Lastly, we observed a doctor interview a patient to learn proper communication techniques. This completely rounded out the day that made med school real. This was a 57 year old woman with bone marrow cancer. She told her story from beginning to end over 45 minutes. It was clear that she placed a lot of trust in Dr. Shochet, and that she respected him. I feel grateful to have these experiences to help me learn how to be a compassionate and competent doctor.
And after a long day, I even got some quality time with my husband! Of course, knowing that I hadn't yet showered after spending a good 4 hours in the anatomy lab, he did say, "Um, you smell a little bad..."
Thursday, August 26, 2010
Abnormalities of the chest
We watched this video in class today! Which was funny... but then I found the surgery to fix it... not as funny, but still fun :)
Wednesday, August 25, 2010
Why am I dissecting a human?
Apparently I should be practicing on a sea turtle.
 Today I used a bone saw to cut through the ribs and sternum and removed the rib cage. We then removed the lungs. Tomorrow: heart.
Today I used a bone saw to cut through the ribs and sternum and removed the rib cage. We then removed the lungs. Tomorrow: heart.
 Today I used a bone saw to cut through the ribs and sternum and removed the rib cage. We then removed the lungs. Tomorrow: heart.
Today I used a bone saw to cut through the ribs and sternum and removed the rib cage. We then removed the lungs. Tomorrow: heart.
Tuesday, August 24, 2010
Anatomy
I did not sleep well last night. Sweat was pouring off of me, I was uncomfortable, and I couldn't stop thinking about what my first day in Gross Anatomy would be like. A human cadaver. Lots of human cadavers in the lab... 24 dead bodies. What would it smell like? Would I be able to cut into the body?
"This will be your first patient. This person wanted you to learn from their body. They will teach you more than any textbook every could." - Dr. T
After a brief lecture about the thorax and what to expect in the thoracic cavity, we changed into our scrubs and headed to lab. The 6 of us stood around our body - it was covered in a green plastic sheet, but I knew underneath was a clear plastic bag, and the body was shrouded in cotton cloth. What parts of the body do we think of as being most "human?" The face. The hands. The feet.
I am nervous, but I am so grateful to have this opportunity, to stand where few can and to learn. My responsibility is to this patient, to my partners, and to my future patients.
"Your responsibility is to learn from this body the things that will help to save the lives of other people." - Dr. K
As a group, a medical team, we started by uncovering the feet and then the hands. We observed the age of the skin and the joints. The coloring was off. Preservatives. You could smell them.
We uncovered the face. This was the strangest thing I've ever done. It wasn't scary, but it was so unusual that it was only natural to feel very uncomfortable. This person is Asian. Small in stature, thick lips, heavy creases around the eyes. I thought about our trip to Thailand, Cambodia and Vietnam - this person could have lived there. It became real.
Our group collectively guessed this person to be a 75 year old male, but after uncovering the entire body we were surprised to find a female. Her knees were bulging: arthritis. She did not have much fat at all - her legs and arms looked pretty good, even toned. Dr. K then reveiled that her age was 91! 91! I hope I look that good at 91!
We broke into our groups of 3 and I stayed to disect the breast, skin and pectoral region with 2 partners while the other group members went to learn about imaging. Then we flip flop. We will do this every day for the next 8 weeks. The three of us will teach the other group what we learn in lab and vice versa. We will all disect every day, for about an hour and a half each day - 3 hours total between both groups. We will learn about the entire body: every organ, muscle, nerve, vessel and bone.
Today we uncovered the pectoral muscles (major and minor) and found lots of great nerves, veins, arteries and connective tissue. We saw the striations of the muscle fibers and found where they connect to the bones.
The pectoralis major connects to the humerus to allow us to lift our arm. It's true. I saw it!
"This will be your first patient. This person wanted you to learn from their body. They will teach you more than any textbook every could." - Dr. T
After a brief lecture about the thorax and what to expect in the thoracic cavity, we changed into our scrubs and headed to lab. The 6 of us stood around our body - it was covered in a green plastic sheet, but I knew underneath was a clear plastic bag, and the body was shrouded in cotton cloth. What parts of the body do we think of as being most "human?" The face. The hands. The feet.
I am nervous, but I am so grateful to have this opportunity, to stand where few can and to learn. My responsibility is to this patient, to my partners, and to my future patients.
"Your responsibility is to learn from this body the things that will help to save the lives of other people." - Dr. K
As a group, a medical team, we started by uncovering the feet and then the hands. We observed the age of the skin and the joints. The coloring was off. Preservatives. You could smell them.
We uncovered the face. This was the strangest thing I've ever done. It wasn't scary, but it was so unusual that it was only natural to feel very uncomfortable. This person is Asian. Small in stature, thick lips, heavy creases around the eyes. I thought about our trip to Thailand, Cambodia and Vietnam - this person could have lived there. It became real.
Our group collectively guessed this person to be a 75 year old male, but after uncovering the entire body we were surprised to find a female. Her knees were bulging: arthritis. She did not have much fat at all - her legs and arms looked pretty good, even toned. Dr. K then reveiled that her age was 91! 91! I hope I look that good at 91!
We broke into our groups of 3 and I stayed to disect the breast, skin and pectoral region with 2 partners while the other group members went to learn about imaging. Then we flip flop. We will do this every day for the next 8 weeks. The three of us will teach the other group what we learn in lab and vice versa. We will all disect every day, for about an hour and a half each day - 3 hours total between both groups. We will learn about the entire body: every organ, muscle, nerve, vessel and bone.
Today we uncovered the pectoral muscles (major and minor) and found lots of great nerves, veins, arteries and connective tissue. We saw the striations of the muscle fibers and found where they connect to the bones.
The pectoralis major connects to the humerus to allow us to lift our arm. It's true. I saw it!
Thursday, August 19, 2010
Bones
This week has been wonderful! I'm having a blast getting to know the amazing, accomplished and impressive students that I'll be learning with over the next 4 years. After taking some time to reflect, I'll write a longer post about the Health Disparities Intersession we've been exploring this week (the health issues in the East Baltimore community, how to think cross culturally, etc)... but I just wanted to mention the box of bones that is now in our living room.

I was planning to walk home on Tuesday, but instead I had to call Matt to come give me and my bones a ride :)

I was planning to walk home on Tuesday, but instead I had to call Matt to come give me and my bones a ride :)
Wednesday, August 11, 2010
Budgets
Following the "Live like a student now" theme, Matt put together a budget and subsequent spreadsheets that will help us follow that budget. We are going to be "proactive" as opposed to "reactive."
 Then he printed them in color and put them on the refrigerator.
Then he printed them in color and put them on the refrigerator.  And apparently they will be updated, printed and re-posted on the fridge each Tuesday.
And apparently they will be updated, printed and re-posted on the fridge each Tuesday.  Ladies, if you can, marry a financial planner.
Ladies, if you can, marry a financial planner.  And if you can't, you can borrow mine for the day. He'll make you nice spreadsheets to keep your spending under control.
And if you can't, you can borrow mine for the day. He'll make you nice spreadsheets to keep your spending under control.
 Then he printed them in color and put them on the refrigerator.
Then he printed them in color and put them on the refrigerator.  And apparently they will be updated, printed and re-posted on the fridge each Tuesday.
And apparently they will be updated, printed and re-posted on the fridge each Tuesday.  Ladies, if you can, marry a financial planner.
Ladies, if you can, marry a financial planner.  And if you can't, you can borrow mine for the day. He'll make you nice spreadsheets to keep your spending under control.
And if you can't, you can borrow mine for the day. He'll make you nice spreadsheets to keep your spending under control.
Subscribe to:
Posts (Atom)